Sympathetic Nerve Fibers
There are many kinds of nerve fibers. Two that are easy to understand are the motor fibers that let us move and the sensory fibers that let us feel. Another important group of fibers that is harder to understand includes the sympathetic nerve fibers.
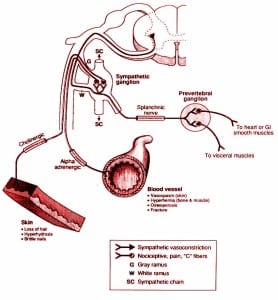
The sympathetic nerves — also called the “C fiber” or “small fiber” nerves — arise from little collections of nerve clusters called ganglia. These are located outside of the spinal cord. The ganglia can function entirely independently (automatically) from the rest of the nervous system.
The sympathetic nerves are of special interest in the study of people who have pain. These nerves are responsible for the kind of pain that is described as burning, achy, tingling, and numbing in character. People who have sympathetic pain often have a hard time describing where their pain begins or ends, but usually can tell you that cold temperatures or shifts in the weather make it worse.
They often describe themselves as naturally having cold hands or cold feet, or may have noticed that since hurting themselves the painful part always feels cold. As it becomes more severe, their skin can become sweaty, and they do not want anyone (or anything) to touch them where they hurt. People who have a “C” or “small” fiber peripheral neuropathy may have these complaints.
In its worst form, sympathetic pain can be very severe. Because it is associated with a change in blood flow and perspiration, the skin can become very thin. While it is the exception and not the rule, in some cases if the individual stops using the painful part, the bone may become very thin as well. Amputation is not unheard of in these less common cases.
Doctors normally refer to severe cases as reflex sympathetic dystrophy. More recently, with the ability of thermography to detect people with sympathetic pain syndromes at an earlier stage, the term sympathetic dysfunction (not responding properly) syndrome has gained popularity.
No one really knows what causes sympathetic pain syndromes, and most doctors are only vaguely familiar with how to diagnose them, let alone treat them. The syndromes are more classically thought of as beginning after relatively minor insult, such as simple ligamentous sprains or from repetitive use injuries.
With a high index of suspicion for the disorder, painful conditions such as post-surgical backs, nerve root irritation, sacroiliac strain, and myofascial syndrome that fail to resolve can be explained. It is in this category that the dysfunction syndromes seem to occur. With more severe injuries (such as fracture) the dystrophy type syndromes occur.
Sympathetic pain syndromes are difficult to diagnose. The most important reason for this is that it is not thought of often enough. The two tests that are used to objectify the presence of a sympathetic pain syndrome are bone scans and thermography. The bone scan is felt to be more specific, but the thermogram is far more sensitive.
Traditionally, the prognosis for the resolution of symptoms with sympathetic pain syndromes is poor. Surgical interventions often worsen the disorder, and as a result treatments usually include the use of physical therapy along with repeated anesthetic blocks (usually of the sympathetic ganglia). More recently, however, there have been some breakthroughs that have improved the chances for a good outcome.
These newer interventions are both diagnostic and therapeutic. Thermography, with its higher sensitivity, allows for an earlier diagnosis. Electric sympathetic analgesia, as compared to the traditional chemical block by injection, has improved patient compliance toward treatment.
At Piedmont Physical Medicine and Rehabilitation we have a high index of suspicion for sympathetic pain syndromes. Rapid diagnosis as well as an aggressive nonsurgical approach is at the cornerstone of our treatment. These interventions enhance our ability to minimize the associated pain and to maximize return to normal function in people afflicted with this syndrome.