Ultrasound Guided Percutaneous Tenotomy
Ultrasound Guided Percutaneous Tenotomy offers a new and innovative technique for treating tendonitis and tendon related pain. With the use of Diagnostic Ultrasound for both localization and needle placement, a percutaneous tenotomy (tendon repair through the skin) can occur. This obviates the need to perform an open procedure (there is no surgical laceration). This outpatient procedure also saves facility and anesthesia related surgical costs.
Excessive repetitive strain of the tendon is thought to be a major influence in the etiology of tendonopathy. Traditionally, tendonosis is thought to occur with overuse, causing microtrauma at a degree and frequency at which the tendon can no longer heal itself. This situation leads to mechanical breakdown of the tendon.
Several authors have studied factors that may influence the development of tendonosis, such as training duration, rest periods, anatomic limb alignment, and mechanical factors related to shoes, inserts, splints, racquets, or clubs. Further confusion arises because tendonopathy also can occur in someone who is relatively inactive. At this time, the exact etiology of tendonosis seems multifactorial, complicated, and incompletely understood.
As with an open surgical procedure, non-surgical treatment options should be considered first. If conservative care — including medications by mouth, rest, splinting, and physical therapy — fails, then ultrasound guided percutaneous tenotomy becomes a viable option. This is especially true in those common cases where complete or severe disruption of the tendon is not present.

With diagnostic musculoskeletal ultrasound, tendonosis (implying non-inflammatory tendon swelling or degeneration) is readily identifiable. After appropriate consent is obtained, the area is properly cleaned and a needle of suitable gauge and length is inserted through the skin. Local anesthetic is injected (making the entire procedure relatively non-painful), and the needle is then advanced through the tendon at its enthesis until it contacts bone. This process is repeated until the enthesis has been pierced by the needle in multiple locations.
Post-procedure intervention includes 24–48 hours of aggressive active range of motion (AROM) exercises, being careful not to use any resistance or add unwarranted load onto the tendon. The moderate use of analgesics such as Ultracet or Darvacet, ice, and electrical stimulation are appropriate as well (most people require only one or two tabs of pain medicine post procedure).
Ideally, a 4–12 week course of physical therapy should be initiated with the goals of improving function, decreasing pain, and increasing strength (without putting the tendon in jeopardy while it is healing). When AROM exercises are faithfully completed, most patients can differentiate between post-procedural pain and their original symptoms within 48 hours. While as many as 15 percent of patients may progress to formal exploration of the tendon, the vast majority report excellent, good or fair results with the percutaneous approach.
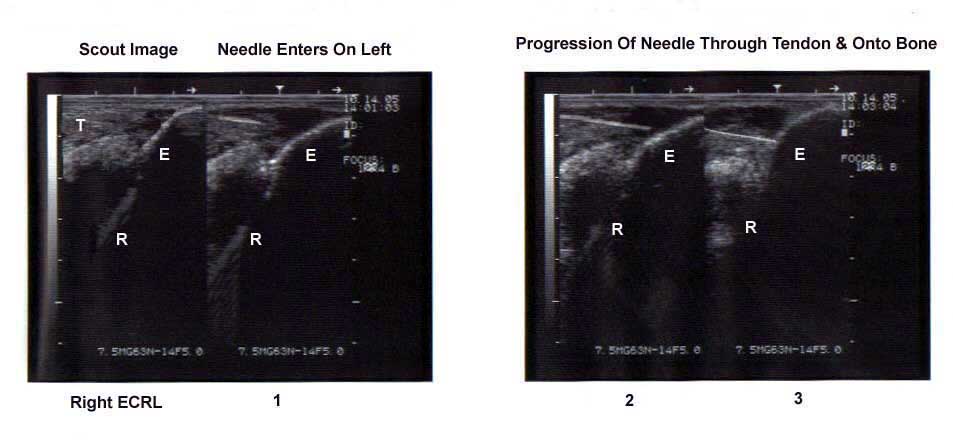
(Needle); T (tendon); E (epicondyle); R (Radius)